The View from the Office
What I’ve Learned in 30 Years of Family Medicine
You can’t prevent 100% of anything. You’re not responsible for guaranteeing anything. Most of the power lies on the patient’s side of the partnership, and a healthy lifestyle is the primary tool. Your job is to help them unleash their power to be healthy.
Health is not freedom from disease. Health is a matter of being aware, content, and eagerly looking forward to the future with whatever physical or emotional limitations you might have and being firmly rooted in your community and your family and committed to their general welfare.
What you really owe your patients is to think for yourself. The experts don’t know your patient, and most of them are paid by a drug company. Your loyalty to your patient is uncompromised. No one knows their details like you do.
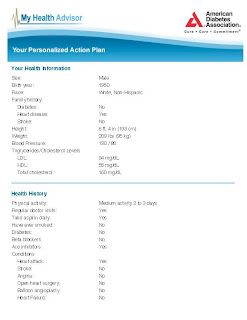
Every visit should be treated as a new patient visit. Going over the family situation, lifestyle score, job, and problem list and medication list should be routine. Just as when you join any practice, every patient is new to you and deserves the same basic intake and assessment from you. These assessments need to be global and represent your best effort to get to know their place in your community. There shouldn’t be any visits where you just treat a cold and let them go. Every visit is an opportunity to get to know them better. Colds don’t matter. Not being thorough just because you’re rushed is a lack of discipline. Discipline is what makes you efficient and keeps you from getting behind in your schedule.
Every visit should start with a conversation about lifestyle. This is, after all, the key to health. Using the formula 0-5-10-30-150 (for 0 cigarettes, 5 servings of fruits and vegetables a day, 10 minutes spent relaxing in some way every day, maintaining a BMI < 30, and getting at least 150 minutes of exercise a week) makes this a simple conversation. Try it. Your patients will respond positively to it.
You can’t beat the 80/20 rule. The 80/20 rule states that 80% of your best results come from just 20% of your best efforts. Medical school curricula were designed by a bunch of obsessive-compulsives who didn’t know a thing about time management. You can’t do everything for every patient. It is pretty easy to identify 80% of traditional practice standards that can just be tossed out. A simple example is the physical exam. What’s a complete physical. Here is my version:
“Vitals reviewed. Constitutional: She is oriented and well-developed, well-nourished, and in no distress. She appears not diaphoretic. No distress. HENT: Head: Normocephalic and atraumatic. Right Ear: External ear normal. Left Ear: External ear normal. Nose: Nose normal. Mouth/Throat: Oropharynx is clear and moist. No oropharyngeal exudate. Eyes: Conjunctivae and extraocular motions are normal. Pupils are equal, round, react to light and accommodate. Right eye exhibits no discharge. Left eye exhibits no discharge. No scleral icterus. Neck: Normal range of motion. Neck supple. No JVD present. No tracheal deviation present. No thyromegaly present. Cardiovascular: Normal rate, regular rhythm and normal heart sounds. Exam reveals no gallop and no friction rub. No murmur heard. Pulmonary/Chest: Effort normal. No stridor. No respiratory distress. She has no wheezes. She has no rales. She exhibits no tenderness. Abdominal: She exhibits no distension and no mass. Soft. No tenderness. She has no rebound and no guarding. Musculoskeletal: Normal range of motion. She exhibits no edema and no tenderness. Lymphadenopathy: She has no significant adenopathy. Neurological: She is alert and oriented. Gait normal. Skin: Skin is warm and dry. No rash noted. She is not diaphoretic. No erythema. No pallor. Psychiatric: Mood, memory, affect and judgment normal.”
This is not a list of the most relevant findings, rather it is evidence of a brief survey of the body that is systematic, easy to perform, and keeps all the Medicare auditors happy. This has the advantage of focusing on the most readily apparent and easy to observe abnormalities; most of the time no abnormalities are recorded for most of the parts of the exam that are done. With repetition this becomes very quick and effortless. My complete physical takes only 2 minutes; problem focused exams take only half that.
The physical exam is only one example. There are many more. Just to take another simple one. Don’t focus on every preventive measure that could possibly be done. This would cost too much in time and money, and since the USPSTF has recommendations for 169 interventions, you would find it just overwhelming. Besides we can’t prevent 100% of anything anyway. The simple rule is to pick up to 7 of your top priorities, and use every visit to make sure they are very well taken care of.
In order to be efficient you have to work in your own way. Any physician who is using a progress note form (whether paper or electronic) that is designed by someone else has been dealt a major blow to efficiency, productivity, and creativity. There is no single common denominator to medical care. The methods of effective practice are as rich and varied as the people who are practicing medicine and the patients who see them. As a craftsman, you are simply negligent if you don’t design your own tools for the way you work. Your efficiency, accuracy, and creativity all depend critically on getting in your groove and just humming along in a way that comes natural to you. Your progress note form should be a brief map for the interaction you want to have with patients. Below is my basic progress note template for both new and established patients, acute or chronic care issues.
It starts with the chief complaint from the patient’s perspective since, if you don’t address this right up front, you have lost their attention and you have missed an opportunity to map your use of time together. Then the very next thing I want to get to is social history where I learn as much about the patient’s milestones through life and role in the community as I can. I spend 2 minutes on completing a lifestyle score using my formula for health (0-5-10-30-150) and remind them how central these 5 behaviors are both to health and the care of any disease. My review of systems includes a search for any and all problems (my note uses a list of the top 16 to prompt me to think of common problems that need not be obvious; you would be amazed at how easy it is to take care of a cold for a patient and not realize that they have cancer) for which the patient has been treated in the past. The added advantage of this is that it expedites your review of chronic diseases giving Medicare the 3 pieces of information they want about at least two each visit (current disease status: whether progressing, improving, or stable; whether it is well-controlled or not; and whether there are any side-effects of treatment); this process also creates a nice mini-report card of the effectiveness of your care.
I also review some basic housekeeping details like whether they need glasses, use hearing aid, have dentures, or need a dental checkup too.
I review what laboratory testing has been done recently and make sure I have values for my top 5—lipid panel, renal function, A1c (if BMI > 30 or have HTN), TSH , and a CBC .
Finally I do my review of my top 5 preventive medicine tasks (lifestyle score [already done], lipid testing, immunizations, Pap and mammogram review for women (particularly noting any past history of abnormals) and offering a PSA test to men, if they want it, and a general discussion (not necessarily any testing) of the pros and cons of colon cancer screening (not essential in my opinion), prostate cancer screening (not recommended), and skin cancer screening. It is worth remembering that a healthy lifestyle avoids more cancer than all of the traditional cancer screening programs put together at a mere fraction of the cost. After that I am just jotting a few notes to myself about abnormalities on exam and the “to do’s” I take away from the visit, and we’re done.
All in all, this is a rich, 15 minute experience that gets the job done. And, of course, I’m not done yet. I hope to get better.
Figure 1: My Basic Progress Note
Visit #: Age: Gender: Name: DOV : 4/21/11
CC:
HPI:
Social: Lives with: Occupation:
Lifestyle score: 0 5 10 30 150
Smoking: Etoh: Known drug issues:
FamHx:
Chronic Problem List:
Status Control Side Effects:
1.
2.
3.
4.
Major 16:
HTN Lipids CAD DM BMI > 30 Smoker CHF
Hx of cancer Depression Hep C Thyroid
BPH Asthma/COPD Afib Warfarin CVA/TIA Chr Pain
GERD Sleep apnea
Surgeries: ________________________________________________________________________
Diabetes: A B C D E F: _______________________________
Major Labs: LDL : (cholesterol) Cr/GFR : (kidney) A1c: (diabetes) TSH : (thyroid) LFTs (liver) PSA (prostate)
Allergies:
Last Pap: Last Mammo: Last colonoscopy: Last PSA : Flu: Last DT Pneumovax Shingles:
Exam: BP: BMI
Other:
Assessment:
Follow-up:
_________________
Creating this global yet intensely targeted health assessment process has been the work of the last 30 years. It takes some experience to get both an adequate perspective (i.e., you can’t worry about every detail) and a confident ability to select what to focus on (that works for you). It takes 30 years to be both relaxed and confident (they don’t naturally go together). Residents starting out in practice are at such a disadvantage in trying to practice good medicine. They are still stuck trying to do it all (impossible), trying to know everything (impossible), trying to keep the experts happy (impossible), and trying to have a life (not quite impossible). Thirty years down the road, one is able to accept that one can neither knows everything nor attends to every detail and one doesn’t give a damn about the alleged experts any more. Moreover, we have a life, for better or worse, the one we made. It is no longer subject to the doubt or speculation that is so distracting to younger physicians. Finally, we are by now firmly entrenched in our communities, and they are taking care of us every bit as much as we take care of them, and the beautiful cycle of nurture completes once again.